What is a Hernia?
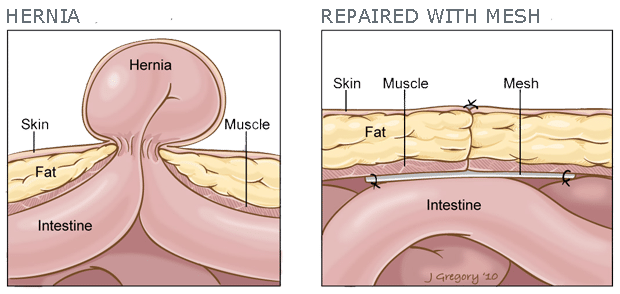
A hernia is an opening or weakness in the wall of a muscle, tissue, or membrane that normally holds an organ in place. If the opening or weakness is large enough, a portion of the organ may be able to push through that area. If you can imagine an inner tube poking through a hole in an old tire – that is what a hernia is like.
Hernias by themselves are not usually life-threatening, but nearly all have a potential risk of having their blood supply cut off, therefore, becoming strangulated. If this happens, it becomes a medical and surgical emergency.
Types of Hernias
These are the most common types of hernias:
Inguinal (groin) hernia: Making up 75% of all abdominal wall hernias and occurring up to 25 times more often in men than women, these hernias occur in the groin area. This hernia gets its name from the inguinal crease which is where the top of the thigh joins the torso.
Femoral hernia: The femoral canal is the path through which the femoral artery, vein, and nerve leave the abdominal cavity to enter the thigh. A femoral hernia causes a bulge just below the inguinal crease in roughly the mid-thigh area.
Umbilical hernia: These common hernias (10% – 30%) are often noted at birth as a protrusion at the belly button (the umbilicus). This type of hernia is more common in women. Umbilical hernias can appear later in life or in women who are having or have had children.
Incisional hernia: Abdominal surgery causes a flaw in the abdominal wall. This flaw can create an area of weakness where a hernia may develop. Even after surgical repair, incisional hernias may return.
What to Expect if Surgery is Required
Dr. Cole will explain the hernia repair surgical procedure in detail before your scheduled surgery. Hernia repairs are performed as an outpatient procedure in a surgery center, and, patients go home the same day.
Post-operative discomfort is usually mild to moderate. Frequently, patients will require pain medication and/or a device called On Q” catheter.
The “On-Q” is a pain relief system designed to provide patients with post-operative pain relief for up to three days (this is separate from the administration of anesthesia for the surgery). Towards the end of the procedure, Dr. Cole will place the On Q” device — a small pump filled with a local anesthetic medication — into the intra-operative site. This device can be removed by the patient on the 3rd day after surgery.
Aftercare should include constant icing of the incision site. This is very therapeutic and hastens recovery.
Dr. Cole will see you in the office one week after surgery and, at that time, will determine the extent of activity including lifting and other forms of physical exertion.